The Current State of Global Liver Health
Known as an organ with over 500 functions, the liver tirelessly works around the clock to maintain the body’s physiology, functioning at full capacity even during sleep. It orchestrates vital processes like detoxification, nutrient metabolism, iron storage, glucose regulation and many others. An interesting corollary to the liver’s importance is its exceptional ability to regenerate to full capacity even if 70-90% of liver tissues are removed. The infamous liver shot can instantly incapacitate even the strongest of fighters, prompting an instinctive curl to shield this vital organ at all costs.
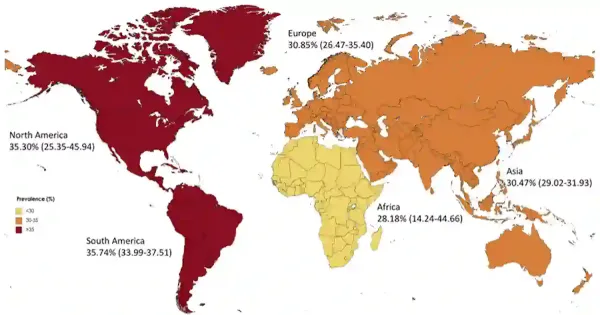
In this era of food overabundance and rising obesity rates, numerous individuals accumulate excessive fat around their livers. Consequently, metabolic dysfunction-associated steatotic liver disease (MASLD), previously called non-alcoholic fatty liver disease (NAFLD), has become the most common liver disorder worldwide. It affects about 30% of the population (Figure 1), regardless of age and body weight. This means even children and lean individuals can develop MASLD. By 2040, the forecasted global prevalence of MASLD stands at a staggering 55%.
Not all cases of NAFLD are life-threatening, however, as this condition varies from basic fatty liver to severe liver scarring called non-alcoholic steatohepatitis (NASH). Currently, NASH is the fastest-growing cause of liver cancer and the reason for liver transplants worldwide. Besides liver cancer, emerging research is starting to link liver health to other types of cancer. This connection is not surprising, given that obesity ranks as the third most powerful modifiable risk factor for cancer. Often accompanying obesity is MASLD, which scientists noted may have obscured the critical contribution of the liver to cancer development.
Figure 1. Prevalence of metabolic dysfunction-associated steatotic liver disease (MASLD), previously called non-alcoholic fatty liver disease (NAFLD), categorised by continent. Source: He et al. (2022), Clinical Gastroenterology and Hepatology.
How Poor Liver Health Drives Cancer
Interestingly, when researchers examined the health outcomes of patients with MASLD, they found that the primary causes of death were not directly related to liver issues but were instead cardiovascular diseases and cancers outside of the liver. A comprehensive meta-analysis of 64 studies calculated that the incidence of non-liver cancers in MASLD patients was 8-fold higher than that of liver cancer (10.6% vs. 1.3% over 10 years). The development of these non-liver cancers did not correlate with MASLD severity, indicating that even patients with mild forms of fatty liver are at an increased risk for these cancers. The most common non-liver cancers found in MASLD patients were those of the breast, prostate, uterus, colon and lungs.
While comparing multiple non-liver cancers to just liver cancer could bias the results towards a higher risk of non-liver cancers, there are underlying mechanisms by which MASLD could foster cancers beyond the liver. One such mechanism was reported in a 2024 study from the University of Hong Kong, showing that fatty livers secrete a pro-cancer hepatokine (hepato- means liver) called hepatic fibroblast growth factor 21 (FGF21). Specifically, excessive FGF21 could upregulate the anti-apoptotic pathways of breast cancer cells, making them more resistant to apoptotic cell death and chemotherapy. This study also found that breast cancer patients with higher levels of FGF21 in their tumour tissues had poorer survival rates and were more likely to experience cancer recurrence than those with lower levels. “Our study emphasises the importance of maintaining liver health in the prevention and treatment of breast cancer, as it reveals the existence of distant crosstalk between the liver and breast cancer,” the study authors concluded.
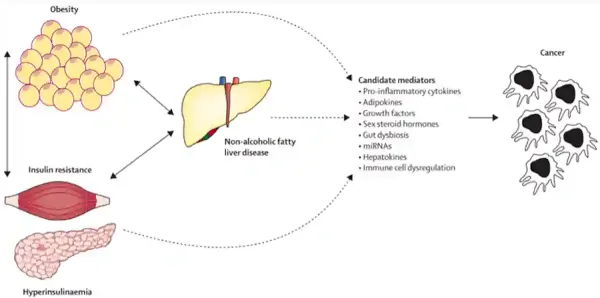
Holistically, MASLD is often viewed in the context of metabolic syndrome, a cluster of conditions involving excessive body fat, hypertension, high blood sugar and high triglycerides. Metabolic syndrome may occur without apparent diseases or alongside diseases like diabetes, obesity and MASLD. Either way, a state of metabolic syndrome triggers chronic inflammation, oxidative stress and insulin resistance through the secretion of pro-inflammatory cytokines and insulin, which are also growth factors for cancer (Figure 2). Liver fat, in particular, has been identified as the greater contributor to systemic inflammation and metabolic syndrome, earning its reputation as the most detrimental form of fat storage compared to other forms of visceral (internal organ) fat.
Additionally, altered levels of sex hormones like estrogen and testosterone in people with metabolic syndrome can encourage the growth of hormone-sensitive cancers, notably breast and prostate cancers. Gut microbiota dysbiosis is also frequently observed in individuals with MASLD and metabolic syndrome, further influencing cancer risk through pathways related to inflammation and immune system dysfunction. By understanding these intricate interactions (Figure 2), it becomes clear that addressing MASLD and metabolic syndrome is paramount in cancer care.
Figure 2. Mechanisms of interorgan crosstalk involving non-alcoholic fatty liver disease (NAFLD), now called metabolic dysfunction-associated steatotic liver disease (MASLD), in the development of cancer, including non-liver cancers. Source: Thomas et al. (2024), The Lancet Gastroenterology & Hepatology.
Strategies to Promote Liver Health
While standard cancer therapies, such as chemotherapy and radiotherapy, are lifesaving, they often overlook the importance of liver health in influencing cancer growth. This oversight likely contributes to the pervasive problems in current cancer care involving high rates of cancer recurrence and therapy resistance. About 80-90% of cancer-related relapses and deaths are attributable to cancer cells evolving resistance to chemotherapy and/or radiotherapy.
However, there are several strategies we can apply to enhance liver health to avoid adding fuel to cancer growth. The surefire yet simplest way is to prevent fat accumulation around the liver through lifestyle habits, such as healthy eating and regular exercise. Medical guidelines for managing MASLD only recommend a weight loss of 5-10% of body weight, as no pharmaceutical drugs have been approved for treating this condition. The use of phytotherapy, i.e., plant compounds with bioactive and therapeutic properties, can also complement this lifestyle approach. Indeed, research has identified several plant compounds that are liver-protective:
- Curcumin (from turmeric): Two clinical trials randomised a group of MASLD patients to lifestyle changes with vs. without curcumin. Results revealed the additional curcumin supplementation decreased liver scarring and blood levels of alanine aminotransferase (biomarker of liver damage) and nuclear factor-kappa B (inflammation biomarker). Studies involving animals also provide cause-and-effect evidence that curcumin can improve liver health and mitigate MASLD severity.
- Lycopene (from tomatoes): A clinical trial involving children with obesity and MASLD showed that calorie restriction with lycopene supplementation was more effective in reducing body weight and liver fat accumulation compared to calorie restriction alone. Another clinical trial demonstrated that lycopene could mitigate inflammatory oxidative damage (measured by biomarkers like malondialdehyde, C-reactive protein and oxidised cholesterol) in adult patients with MASLD.
- Genistein (from soy): In a clinical trial of MASLD patients undergoing lifestyle changes, additional genistein supplementation managed to lower blood levels of insulin, pro-inflammatory cytokines and oxidative molecules compared to placebo. A new clinical trial in 2024 confirmed genistein’s benefits in reducing blood triglycerides, cholesterol levels, and waist and hip circumference in patients with metabolic syndrome.
- Quercetin (from fruits and onions): Another 2024 clinical trial reported that MASLD patients who received quercetin supplementation had a greater reduction in liver fat content and body weight compared to those on placebo. Research in animal models of MASLD showed that quercetin could activate signalling pathways for autophagy (i.e., self-cleaning system) to lower inflammation and improve liver health (Figure 3).
Notably, these plant compounds are also included in our Pfeifer Protocol, which capitalises on phytotherapy to provide complementary and personalised treatment to enhance the quality of life and condition of cancer patients. While standard cancer therapies are invaluable, their limited ability to improve liver health highlights the necessity for a holistic approach to cancer care. This includes educating patients on lifestyle modifications and complementary therapies to provide a more integrative care plan, which addresses all aspects of patient health.
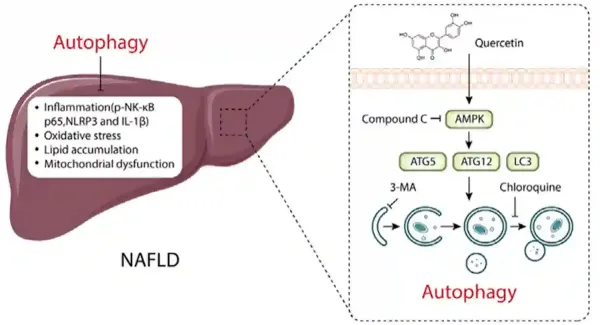
Figure 3. Molecular mechanism of quercetin in treating non-alcoholic fatty liver disease (NAFLD), now called metabolic dysfunction-associated steatotic liver disease (MASLD). Source: Cao et al. (2023), The Journal of Nutritional Biochemistry.