Did you know that by the age of 60, about half of men will experience the symptoms of an enlarged prostate, a condition known as benign prostatic hyperplasia (BPH)? Imagine waking up multiple times a night with an urgent need to urinate, only to feel like your bladder is not empty because an enlarged prostate is blocking the flow of urine. For millions of men, BPH brings sleepless nights, discomfort and a search for effective solutions. Our current newsletter trilogy aims to guide men with BPH through their journeys. In this first part, we will cover the basics – the symptoms, risk factors and, most importantly, treatment strategies of BPH.
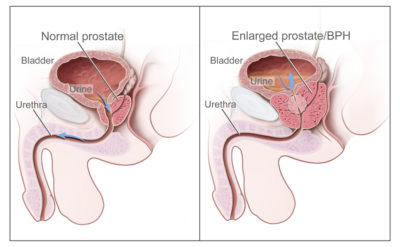
BPH is a non-cancerous condition where the prostate gland enlarges. While its exact cause remains unclear, BPH is thought to result from a combination of age-related hormonal shifts, immune system changes, and natural cellular wear and tear. The prostate, an almond-shaped gland responsible for producing seminal fluid, surrounds the urethra. When it enlarges, the prostate can compress the urethra (Figure 1) and cause unpleasant urinary symptoms:
- Increased frequency of urination, particularly at night (nocturia).
- Difficulty initiating urination.
- Weak urine stream and dribbling at the end of urination.
- Sensation of incomplete bladder emptying.
Symptoms of BPH begin subtly – a weaker urine stream or the occasional extra trip to the bathroom. Over time, these symptoms can get progressively worse and begin to impair one’s quality of life. For example, frequent night-time urination (nocturia) disrupts sleep, leading to fatigue and emotional distress, while the constant need to find a bathroom can interfere with daily activities and social interactions. In severe cases, BPH can cause acute urinary retention, an emergency condition where one cannot urinate despite a full bladder. Other medical complications may also arise from untreated BPH, such as bladder stones, urinary tract infections and kidney damage due to the strain placed on the urinary system.
Figure 1.Normal versus enlarged prostate. The left panel shows the normal flow of urine from the bladder through the urethra. The right panel shows an enlarged prostate pressing on the bladder and urethra, blocking the flow of urine. Source: Public Domain.
The prevalence of BPH increases with age. Autopsy research has observed enlarged prostate in about 50% of men aged 51-60 and up to 90% of men older than 80. This high prevalence makes BPH the most common prostate complication in men over 50. However, not all men face the same risk. Factors that increase the risk of BPH include:
- Ageing: The prostate naturally enlarges at a rate of 0% to 3.5% per year in men, largely due to age-related hormonal changes. As testosterone levels decline faster than oestrogen, the relative increase in oestrogen activity may stimulate prostate growth. The accumulation of dihydrotestosterone (DHT), a derivative of testosterone, during ageing can also promote the growth of prostate cells.
- Family History: Men with a first-degree relative, such as a father or brother with BPH, are 4-fold more likely to develop the condition compared to men without such a family history. Advanced genomic analyses have also pinpointed several immune-related genes (e.g., BTN3A2 and C4A) linked to an elevated risk of BPH.
- Metabolic Syndrome: Metabolic syndrome – a cluster of conditions including obesity, hypertension and insulin resistance – is widely linked to larger prostate volumes and to BPH. Proposed mechanisms include chronic inflammation and higher oestrogen activities, both of which may promote prostate enlargement. Poor glucose control has also been correlated with more severe BPH symptoms.
- Poor Lifestyle: Diets high in red meat and low in vegetables have been associated with a 30-40% higher risk of BPH. Other lifestyle factors linked to BPH include micronutrient deficiencies, physical inactivity and smoking.
Understanding the symptoms and risk factors of BPH is key to recognising the condition early and preventing its progression. The good news is that BPH is manageable, particularly when detected early. A range of strategies, including lifestyle modifications, medications and surgical interventions, can effectively alleviate symptoms and improve quality of life.
For men with mild BPH symptoms, clinical guidelines recommend watchful waiting combined with lifestyle adjustments, such as:
- Moderating fluid intake, especially in the evening, to reduce nocturia.
- Avoiding bladder irritants like caffeine and alcohol.
- Maintaining a healthy weight and exercising regularly.
- Limiting the intake of salt.
- Pelvic floor exercises (Kegels) to improve bladder control.
As many as 70-90% of men with mild BPH will not experience drastic disease progression, indicating that medical interventions may not be necessary. However, regular reassessments, typically annually, are still recommended to monitor symptoms and disease progression. This active surveillance approach mirrors strategies used in prostate cancer management, focusing on symptom control while avoiding unnecessary treatments and their associated risks.
For men with moderate to severe BPH, medications may be necessary to alleviate symptoms. These include α-adrenergic blockers or phosphodiesterase-5 inhibitors that relax smooth muscles, which reduce tension in the prostate and bladder to improve urinary flow. Another option is 5α reductase inhibitors, which block the conversion of testosterone into DHT (i.e., a hormone that can stimulate prostate cell growth). However, these medications can bring side effects in some cases: smooth muscle relaxants can cause headaches, low blood pressure (hypotension) and nasal congestion, while DHT inhibitors can lead to erectile dysfunction, breast enlargement (gynecomastia) and decreased ejaculation.
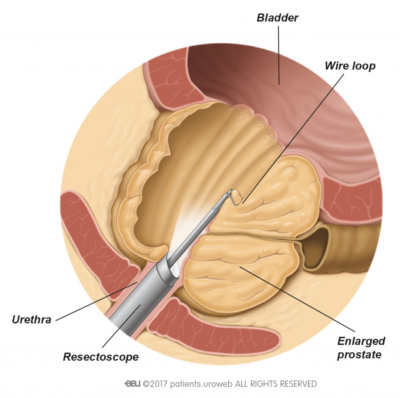
Surgery is then recommended for men who do not respond well to medications or develop severe complications such as bladder stones, urinary retention or kidney failure. The gold standard method is transurethral resection of the prostate (TURP), which involves inserting a resectoscope with a camera and wire loop to cut excess prostate tissue in small pieces to relieve obstruction (Figure 2). While it provides long-term relief, TURP carries risks like retrograde ejaculation (where semen enters the bladder instead of exiting through the penis), urinary incontinence (loss of bladder control) and erectile dysfunction. Despite these risks, TURP remains a widely performed and successful treatment for men with severe BPH.
Figure 2.Transurethral resection of the prostate (TURP). Source: EAU Patient Information, European Association of Urology (EAU).
For patients seeking less invasive options, alternatives to TURP have become increasingly popular due to their shorter recovery times and lower risk of complications:
- Laser therapies use high-energy lasers to target and vaporise excess prostate tissue.
- Water vapour therapy uses thermal energy from water vapour to shrink prostate tissue.
- Prostatic urethral lift places small implants to hold the prostate tissue away from the urethra, relieving obstruction without removing tissue.
While these alternatives are less invasive, they may not be suitable for all patients. Their availability is often limited to specialised centres, and their long-term outcomes may not yet match the well-documented durability of TURP. Some patients may require repeat procedures over time, particularly in cases of prostatic urethral lift or water vapour therapy. The choice of procedure also depends on individual factors. For example, laser therapies are more effective for men with larger prostates or taking blood-thinning medications, whereas prostatic urethral lift is better suited for younger patients who want to avoid complications like retrograde ejaculation. Ultimately, these minimally invasive surgical alternatives allow men with BPH to choose procedures that align with their needs, health status and lifestyle considerations.
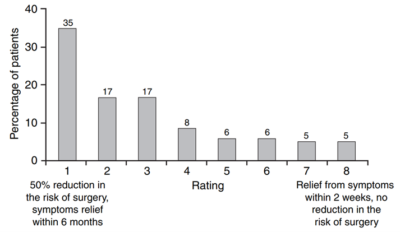
Despite the range of available treatments, many men with BPH remain dissatisfied. A survey conducted across five European countries revealed a disconnect between patient priorities and physician approaches to treating BPH. While most physicians prioritise immediate symptom relief, over 70% of patients reported they would prefer drugs that lower the risk of needing surgery and long-term complications over drugs that offer rapid symptom relief (Figure 3). Similar findings were reported by studies of British and American populations, suggesting that this misalignment is widespread across healthcare systems.
Figure 3. Patient preferences for drug attributes rated on a scale of 1-8. A score of 1 represents a drug that reduces the risk of surgery by 50% with symptom relief starting within 6 months; a score of 8 represents a drug offering rapid symptom relief within 2 weeks but no reduction in the risk of surgery. The majority (77%) rated ≤4, indicating a preference for a drug that prioritises long-term rather than short-term outcomes. Source: Emberton et al. (2008), The International Journal of Clinical Practice.
This dissatisfaction is further compounded by the stigma surrounding urinary issues, which are usually perceived as a private matter. As a result, many men feel reluctant to discuss their condition, leading to underreporting and delays in seeking medical care. Therefore, public health campaigns aimed at destigmatising BPH and increasing awareness of available therapeutic options are imperative to encouraging earlier interventions.
More concerningly, current discourse often overlooks the impact of BPH on the quality of life. Beyond urinary symptoms, BPH frequently causes disrupted sleep, reduced productivity, fatigue, emotional distress and self-esteem issues. Many men also report challenges in maintaining healthy relationships and social life, as the condition can bring embarrassment and anxiety about managing symptoms in public settings. Yet, these non-urinary symptoms are rarely addressed in standard treatment protocols, leaving many patients feeling unsupported.
Overcoming these challenges requires a shift toward patient-centred care, emphasising holistic strategies that go beyond immediate urinary symptom relief. In the next newsletter, we will explore the potential of natural remedies to nurture not only prostate health but also overall well-being. Our ultimate goal is to optimise personalised care strategies that address the unique needs of every patient and empower them to reclaim control over their health.