We trust computed tomography (CT) scans to diagnose conditions and save lives, but what if they are quietly fuelling a future wave of cancers? A new study warns that the soaring use of CT imaging in the U.S. could lead to over 100,000 additional cancer cases decades later – enough to account for 5% of all future diagnoses – driven solely by the radiation exposure patients receive. Given these findings, experts are urging a hard look at how often and safely we turn to this powerful technology in everyday medical care. This newsletter will explore the scientific rationale linking CT scans to cancer, examine the latest risk projections, and explore what can be done to reduce harm without sacrificing diagnostic precision.
CT Scan and Cancer Risk: Theoretical Concerns
When computed tomography (CT) scans first entered clinical practice in the 1970s, doctors were able to peer inside the human body with unprecedented clarity for the first time. As a result, internal tumours, infections, blood clots and injuries can be detected without cutting open the body. At the time, few questioned the risks. Unlike therapeutic radiation (i.e., cancer radiotherapy), the doses delivered by CT were viewed as small and safe.
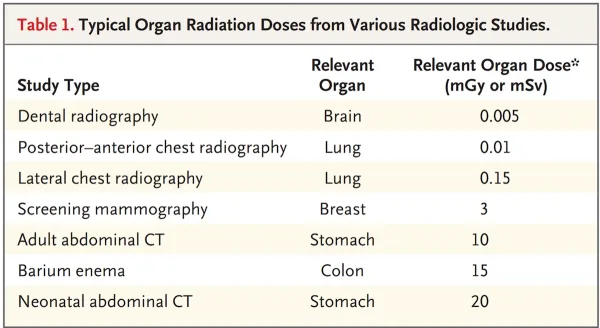
Over time, however, concerns about the safety of CT scans began to surface, especially when CT uses a radiation dose of 10 to 1000 times higher than standard X-rays (Figure 1). An X-ray takes a quick, flat snapshot of the body, while a CT scan creates a detailed 3D image using many X-rays. Although most radiation-induced damage to our DNA is rapidly repaired, sometimes these repairs can go wrong and cause cancerous mutations. Radiation’s carcinogenic effects are thought to be ‘stochastic,’ which means no safe threshold exists. Even low doses could theoretically trigger cancer risk, with the odds rising as the dose increases.
Figure 1. A table detailing the radiation dose an organ receives from various radiologic sources. Standard X-ray radiography (e.g., dental radiography, posterior-anterior or lateral chest radiography, and mammography) uses minimal radiation doses (0.005 to 0.15 mSv) compared to a typical abdominal CT scan (10 to 20 mSv). Source: Brenner and Hall (2007), The New England Journal of Medicine.
The strongest evidence linking radiation exposure to cancer comes from longitudinal studies of Japanese atomic bomb survivors, who were exposed to much higher doses of radiation at over 100 mSv. In comparison, a CT scan typically directs a radiation dose of 15 to 30 mSv to the organ, which may still carry a small risk of cancer. “There was a significant increase in the overall risk of cancer in the subgroup of atomic-bomb survivors who received low doses of radiation, ranging from 5 to 150 mSv,” mathematicians and radiologists David J. Brenner and Eric J. Hall wrote in a 2007 paper in The New England Journal of Medicine, a world-leading journal. “The mean dose in this subgroup was about 40 mSv, which approximates the relevant organ dose from a typical CT study involving two or three scans in an adult.”
More evidence of radiation-induced cancer risk comes from nuclear industry workers. In a major multinational study of over 400,000 workers across 15 countries, researchers found that the risk of dying from cancer increased by about 10% for every 100 mSv of radiation exposure. The study also showed a clear, dose-dependent relationship between radiation exposure and cancer mortality, mirroring patterns seen in survivors of the atomic bomb. This finding reinforces the theory that radiation doses raise cancer risk in a linear fashion. Following this, every 10 mSv of radiation could theoretically raise the risk of cancer mortality by about 1%. In fact, the nuclear workers in the study received an average of about 20 mSv over their careers, a level of exposure similar to CT scans, particularly abdominal or chest CT.
Notably, the risk of radiation-induced cancer is more pronounced in children. Compared to adults, children’s developing tissues divide more rapidly, making them more vulnerable to radiation-induced DNA damage and mutations. As children also have a longer remaining lifespan, they have more time for radiation-initiated cancer to develop and manifest. “In summary, there is direct evidence from epidemiologic studies that the organ doses corresponding to a common CT study (two or three scans, resulting in a dose in the range of 30 to 90 mSv) result in an increased risk of cancer,” Brenner and Hall continued. “The evidence is reasonably convincing for adults and very convincing for children.”
CT Scan and Cancer Risk: What the Latest Data Says
Early estimates from researchers at the University of Oxford, U.K., suggested that CT imaging accounted for just about 0.2% of all cancer cases in the U.K. in the 1990s. Building on this, Brenner and Hall later projected that – as CT use in the U.S. soared to nearly ten times the rate seen in the U.K. – CT scans could eventually contribute to as much as 1.5% to 2% of all cancer cases in the U.S. Consequently, a modelling study calculated that about 29,000 future cancer cases could be attributed to CT scans performed in the U.S. in 2007 alone, with the greatest risk seen among adults aged 35–54 years undergoing abdominal or pelvic CT scans.
Fast forward to today, CT has become deeply embedded in routine medical care. The global usage rate of CT has soared over 30% since the 1990s, with a steady 3–4% increase annually. As a result, recent data warns that the future cancer burden from CT imaging could be far higher than early projections anticipated. Specifically, an updated modelling study from the University of California, San Francisco, estimated that approximately 103,000 future cancers could be linked to CT scans performed in the U.S. in 2023 alone.
Newly published in JAMA Network, this updated study analysed real-world data from over 93 million CT scans across 62 million patients in the most comprehensive modelling to date. They first estimated the radiation absorbed by different organs for each type of CT scan, a process known as radiation dose reconstruction. These dose estimates were then fed into a sophisticated cancer risk calculator developed by the U.S. National Cancer Institute, which accounts for factors like age, sex, organ sensitivity and life expectancy to estimate how many people might eventually develop cancer in their lifetime because of radiation exposure.
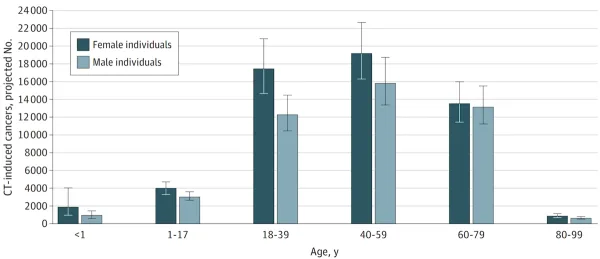
While the individual risk of developing cancer from a single CT scan remains small, the sheer volume of scans performed each year magnifies the overall impact at a population level. The greatest contributors to the projected cancer burden were abdominal and pelvic CT scans in adults, followed by chest CT scans. Lung, colon and blood cancers were among the most common types projected in adults. In children whose developing tissues are more sensitive to radiation, thyroid and breast cancers were predicted to be more common. Although cancer risk per scan was highest in children, the majority of projected CT-related cancers came from adults simply because adults undergo CT imaging far more frequently due to the higher prevalence of chronic diseases or medical conditions requiring CT scans (Figure 2).
Figure 2. Total projected lifetime cancers by sex and age at exposure to computed tomography (CT). Source: Smith-Bindman et al. (2025), JAMA Network.
If current patterns of CT use and radiation dosing continue unchanged, the study warns that CT scans could eventually account for up to 5% of all new cancer diagnoses in the U.S. each year, a figure comparable to other major risk factors like alcohol consumption and excess body weight. That said, most of the projected cancers will not appear immediately; they are expected to emerge around 10 to 40 years later, since radiation-related cancers have a long latency period. Put simply, the sheer amount of CT scans currently conducted in the U.S. alone will likely contribute to a rise in cancer cases sometime between 2033 and 2073.
Since the cancer risk from a single CT scan is small at the individual level, it would require following millions of people over several decades to detect a clear signal, which is extremely difficult and costly to do in real life. As a result, scientists currently rely on risk models rather than waiting for long-term epidemiological data. These models are built using the best available evidence, especially from survivors of the atomic bomb and nuclear workers, whose experiences have provided important insights into how radiation causes cancer.
“CT is frequently lifesaving, yet its potential harms are often overlooked, and even very small cancer risks will lead to a significant number of future cancers given the tremendous volume of CT use in the United States,” the study authors wrote. “For current utilisation and radiation dosing practices, we projected approximately 103 000 future cancers could result from CT use in the United States in 2023 (with sensitivity analyses projecting a range of 80 000 to 127 000) among the 62 million people who underwent CT.”
CT Scan and Cancer Risk: How Can We Minimise Risks?
CT scans can be lifesaving when used appropriately, but minimising the risks of radiation-induced cancer requires prudent decision-making. As a result, many expert and regulatory bodies have published guidelines on when a CT scan is warranted.
The first and most effective way is to scan only when necessary. Sometimes, doctors may order scans just to be extra cautious, i.e., to avoid missing a rare diagnosis or legal repercussions if something is overlooked – a practice known as defensive medicine. Imaging may also be repeated because a previous scan was not sent properly from another hospital, or the quality was poor. As a result, some hospitals have implemented electronic systems to flag low-value imaging requests, which refer to scan requests that offer little to no clinical benefit. Nevertheless, not all hospitals use these systems. Studies still suggest that about 30% of CT scans may not meet evidence-based guidelines.
Second, CT scanners can often be adjusted to use less radiation, especially in smaller patients. Newer machines use advanced software like adaptive statistical iterative reconstruction (ASIR), which allows high-quality images to be produced using lower radiation doses. However, not all facilities have adopted these upgrades. Another problem is multiphase scanning, when the same area is imaged multiple times in rapid succession. While this can be useful for certain complicated conditions, it often results in radiation doses 2–4 times higher than a standard CT scan. Experts, therefore, suggest that certain multiphase CT scans could be replaced by magnetic resonance imaging (MRI) without compromising accuracy.
Third, precautions must be taken for individuals at greater risk of radiation-induced cancer. Children are especially vulnerable because their developing tissues are more radiosensitive and they have many more years ahead for a cancer to develop. Women are also at greater risk due to their higher baseline risk of breast and lung cancers. Pregnant patients require additional caution: while CT scans of the head or limbs are safe, abdominal or pelvic CT scans can expose the foetus to radiation. Additionally, patients with a high body mass index (BMI) often receive greater radiation doses because more energy is needed to penetrate thicker tissues.
Fourth, radiation doses can vary dramatically from one facility to another, even for the same type of CT scan. Published analyses have found as much as a 13-fold variation between the highest and lowest doses used across hospitals. So, experts advise choosing accredited imaging centres, which are required to meet certain safety standards and undergo regular dose audits. When in doubt, patients (and referring doctors) should ask whether a facility follows dose-limiting protocols or uses low-dose CT technologies.
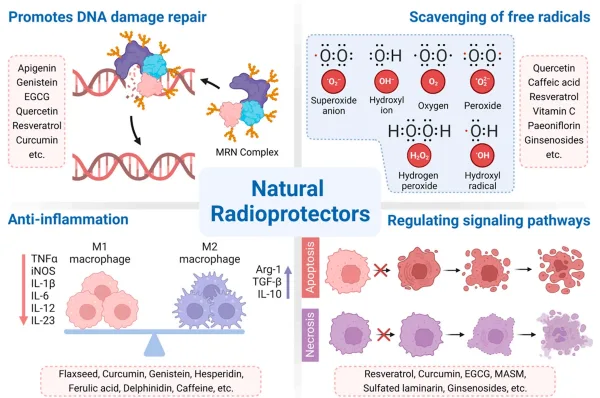
Fifth, it may also be worth considering phytotherapy (plant-based) approaches to reduce the cancer risk associated with CT scans. Several plant-derived compounds (e.g., curcumin, resveratrol, quercetin, and green tea catechins) have demonstrated radioprotective effects in laboratory studies. Specifically, these compounds can facilitate the repair of DNA breaks by activating DNA repair enzymes and suppressing oxidative stress (Figure 3). However, their efficacy in protecting human tissues from the lower radiation doses from CT scans remains unproven. For now, such phytotherapy strategies are best seen as complementary to, and not replacements for, safer scanning practices.
Figure 3. An overview of the radioprotective properties of plant compounds. For example, green tea catechins (EGCG), quercetin, resveratrol and curcumin are some of the plant compounds capable of promoting DNA damage repair. Source: Zhang et al. (2023), Cancers.
Ultimately, the story of CT imaging is one of remarkable progress shadowed by quiet risk: the very technology that helps us detect disease may, in the long run, contribute to it. As our diagnostic technology advances, so does our responsibility to use it wisely by choosing when, how and whom to scan. If we fail to recognise the potential long-term harm of diagnostic radiation today, we may face a slow-boiling public health problem decades later.