New Data
Breast cancer must not be taken lightly. In 2020, breast cancer overtook lung cancer as the most common type of cancer worldwide. That year, we witnessed a staggering 2.3 million new cases and 685,000 deaths from breast cancer alone. By 2040, a statistical study estimated an increase of over 40% in new breast cancer cases, coupled with more than 50% rise in breast cancer fatalities (Figure 1). Both the present and future of breast cancer seem bleak.
Figure 1. Estimated number of breast cancer cases and deaths from 2020 to 2040, according to the level of Human Development Index (HDI), a measure of the overall country development based on indicators such as life expectancy, education, and income. Source: Arnold et al. (2020), Breast.
A new study, however, delivers a glimmer of optimism – that there is a way to halve the risk of breast cancer. The study, published earlier this year in BMC Women’s Health, was conducted by scientists from Tehran University of Medical Sciences, Iran’s highest-ranked research institution. This study recruited 150 women with breast cancer, alongside 150 healthy women of similar age who were relatives of the breast cancer patients. Using relatives as the control group helps to minimise the effect of confounding variables, such as socioeconomic and genetic differences, potentially skewing the study results.
That said, the study revealed two key results:
- Women in the top 25% quartile of adherence to the Mediterranean diet were 55% less likely to develop breast cancer than women in the lowest 25% quartile. This effect remained significant after adjusting for potential confounders, such as education, family history of breast cancer, physical activity, marital status, smoking, and energy intake.
- Such protective effects of the Mediterranean diet were stronger in post-menopausal women, with a significant 76% reduction in odds of breast cancer in those in the highest vs. lowest quartile of Mediterranean diet adherence.
The first point is particularly crucial. It indicates the Mediterranean diet is solely responsible for lowering the odds or risk of breast cancer, independent of other variables. This also means that every woman can benefit from this diet, regardless of her age, genetics, exercise levels, etc.
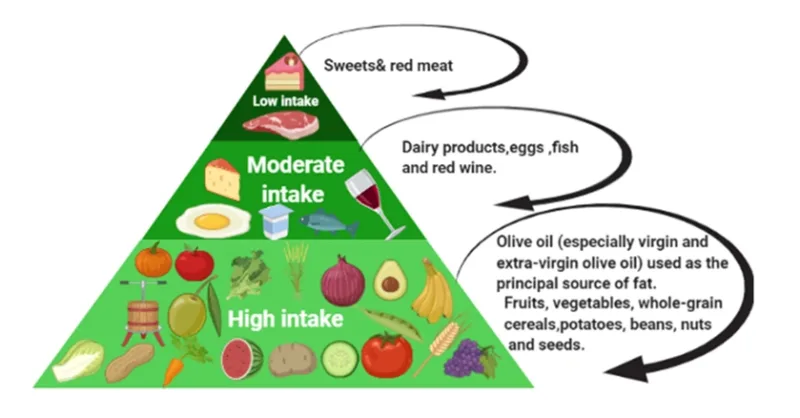
Finally, the study authors attributed the protective effects of the Mediterranean diet against breast cancer to the high amounts of vegetables, fruits, whole grains, nuts and olive oil present in the staples of the diet (Figure 2). A wealth of existing research has shown that these plant-based foods are rich in compounds exhibiting potent anti-cancer effects. Armed with this knowledge, the Pfeifer Protocol capitalised on these plant-derived compounds to combat cancer, as the next section describes.
Figure 2. Mediterranean diet intake level. Source: Mahmod et al. (2022), Frontiers of Nutrition.
The Pfeifer Protocol
To recapitulate, a recent study from a leading Iranian research institution has demonstrated that the Mediterranean diet high in plant-based foods is highly effective at lowering the risk of breast cancer by as much as 55%. This finding further affirms the validity of the Pfeifer Protocol, developed to safeguard against such hazards using personalised, evidence-based phytotherapy.
For individuals at risk of breast cancer, such as those having a family history of breast cancer, the Pfeifer Protocol recommends:
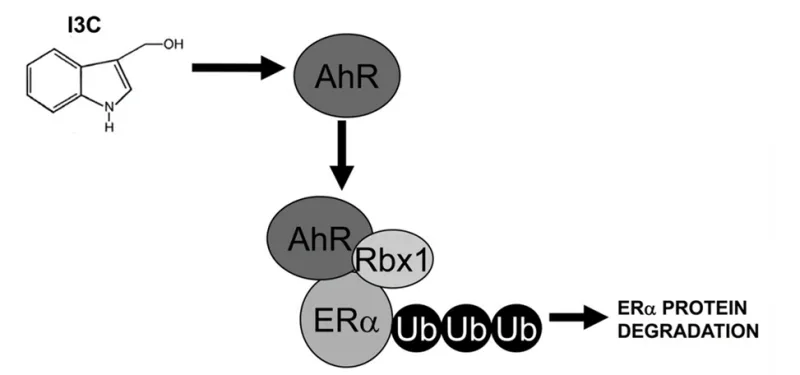
- Indole-3-Carbinol (2×1 capsule daily): a glucosinolate derivative of cruciferous vegetables, which is a known regulator of oestrogen metabolism important for breast health.
- IMUSAN (2×1 capsule daily): a blend of 15 plant extracts that bolsters the overall immune system, including immune cells imperative for inhibiting cancer development.
- BioBran (2×1 sachet daily for the first month, then 1×1 daily): an arabinoxylan compound derived from rice bran, which possesses immune-enhancing and anti-cancer properties.
However, the absence of a family history of breast cancer does not guarantee immunity to the disease. In fact, 80-85% of breast cancer patients do not have a family history of the disease. The above recommendations may also be applied for those without such apparent genetic risk, although BioBran may not be necessary. This is because the function of indole-3-carbinol and IMUSAN in supporting oestrogen and immune regulation are still beneficial for healthy women (Figure 3).
Figure 3. Indole-3-carbinol (I3C) regulates oestrogen metabolism. Specifically, I3C activates the aryl hydrocarbon receptor (AhR) to initiate Rbx-1-mediated ubiquitination (Ub) and degradation of oestrogen receptor alpha (ERα) in breast cancer cells. Overactive ERα is known to drive the development and growth of breast cancer. Source: Marconett et al. (2010), Molecular Biology of the Cell.
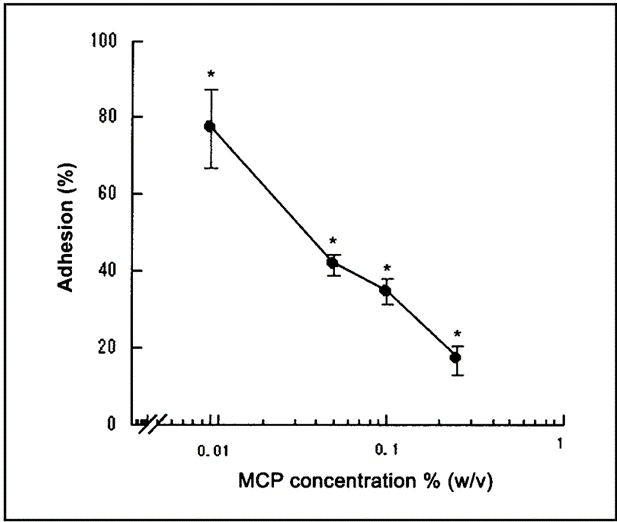
Depending on the patient’s situation, the above recommendations can still be modified further. For instance, for breast cancer patients who completed therapy but want to avoid cancer recurrence, we may introduce Aeskulap-Modified-Citrus-Pectin, which prevents cancer cells from latching onto healthy tissues by blocking the galectin-3 receptor (Figure 4). Variations of the Pfeifer Protocol are also available for those with ongoing or recurrent breast cancer, as well as those with scheduled breast tissue biopsy but wish to minimise the small risk of the biopsy needle dislodging cancer cells from the tumour and seeding tumour growth elsewhere.
Evidently, the Pfeifer Protocol merges a range of specially crafted plant-derived compounds that aim to prevent and combat cancer, including the widespread breast cancer. As such, patients do not have to adhere sternly to the Mediterranean diet or consume excessively large quantities of fruits and vegetables to gain comparable anti-cancer benefits.
Figure 4. Modified citrus pectin (MCP) decreased the adhesion of breast cancer cells to nearby blood vessels by inhibiting the galectin-3 receptor in a dose-dependent manner. Source: Nangia-Makker et al. (2002), Journal of the National Cancer Institute.
Closing Remarks
Despite groundbreaking strides in medical technology, the incidence and mortality of breast cancer patients are rising at an alarming rate, and projections suggest this trend is far from over (Figure 1). Scientists attribute this statistical increase due to the growing prevalence of:
- Reproductive risk factors: e.g., advanced age at first birth and less breastfeeding.
- Hormonal risk factors: e.g., hormone-replacement therapy and oral contraceptives.
- Behavioural risk factors: e.g., alcohol consumption, physical inactivity and poor diet.
Given the multifactorial determinants of breast cancer, no single solution exists for breast cancer prevention. Still, we are not powerless in this matter. We can take significant steps to mitigate the risk of breast cancer, be it by adhering to the Mediterranean diet or recommendations of the Pfeifer Protocol.
As the old cliché goes, prevention is better than treatment. But let us take it a step further. We must remember that knowledge is power, and understanding the risks and preventative measures of breast cancer empowers us to face the future not with fear, but with preparedness and commitment to our health. Every step we take towards prevention is a victory against breast cancer. We do not have to let grim statistics dictate us.